Marijuana legalization: Where the debate stands
Reading Time: 9 minutes The debate on marijuana legalization continues: Here’s what we know about the pros and cons
Reading Time: 9 minutes The debate on marijuana legalization continues: Here’s what we know about the pros and cons
Reading Time: 6 minutes By now, many of us probably know someone who’s been affected by opioid addiction. Learn how to spot the signs of an overdose and where to get help.
Rate this article and enter to win
What do you know about opioid abuse and addiction? Take our quiz to see how your knowledge compares to other students’, and find answers to questions like these:
The US is experiencing a brutal opioid epidemic. In 2015, 33,000 Americans died from overdoses involving prescription painkillers, heroin, and synthetic opioids, according to the National Institutes of Health. Many opioid overdoses can be reversed with timely medical treatment, however—someday, you may be in a position to save a life. This brief guide shows you how.
The illicit use of heroin and prescription painkillers is rare among college students. Yet this epidemic is affecting demographics that were previously considered relatively immune to drug crises. “My freshman year of college, my older sister went to rehab for heroin addiction. People from all ethnicities and social classes are struggling with opioid addiction,” says a third-year undergraduate at Saint Louis University, Missouri.
In this article, “opioid” covers heroin, prescription painkillers, and synthetic opioids sold on the street. For info on getting help with abuse and addiction, see Get help or find out more.

» The signs of opioid overdose include:
» As the window for intervening narrows, signs include:
Opioid addiction is difficult to treat. Avoiding illicit drug use is the safest strategy. Here’s how to look out for yourself:
Many opioid overdoses can be reversed with treatment. The opioid reversal medications naloxone and naltrexone can be delivered via a nasal spray, by injection, or intravenously. These reversal drugs (or antidotes) are also known by various brand names (e.g., Narcan®).
Naloxone treatment can be accessed in several ways:
Here’s what being unresponsive looks like, according to the Harm Reduction Coalition:
See Where can I get help with opioid abuse or addiction? in the article.
How to respond to an opioid overdose: Harm Reduction Coalition
Does your state have a “Good Samaritan” law [pdf]: Drug Policy Alliance
Interactive guide to the opioid epidemic: Guardian
Find treatment near you: Substance Abuse and Mental Health Services Administration (SAMHSA)
Free, confidential, 24/7 helpline (English and Spanish): SAMHSA
1-800-662-HELP (4357)
1-800-487-4889 (TDD)
Find a local meeting: Narcotics Anonymous
Guide to drug addiction treatment: National Institute on Drug Abuse
Facts about heroin: Drug Policy Alliance
Can you get over an addiction? Maia Szalavitz/New York Times
Achilefu, A., Joshi, K., Meier, M., & McCarthy, L. H. (2017). Yoga and other meditative movement therapies to reduce chronic pain. Journal of the Oklahoma State Medical Association, 110(1), 14–16.
American College Health Association. (2016). American College Health Association-National College Health Assessment II: Reference Group Executive Summary, Spring 2016. Hanover, MD: American College Health Association; 2016.
Arnold, R. (2017). Fast Facts and Concepts #83. Why patients do not take their opioids. Palliative Care Network of Wisconsin. Retrieved from https://www.mypcnow.org/blank-aw14v
Back, S. E., Payne, R. L., Wahlquist, A. H., Carter, R. E., et al. (2011). Comparative profiles of men and women with opioid dependence: Results from a national multisite effectiveness trial. American Journal of Drug and Alcohol Abuse, 37(5), 313–323.
Brooner, R. K., King, V. L., & Kidorf, M. (1997). Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. JAMA Psychiatry, 54(1), 71–80.
Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51).
Centers for Disease Control and Prevention. (2012). Grand Rounds: Prescription drug overdoses—a US epidemic. Morbidity and Mortality Weekly Report, 61(1), 10–13.
Centers for Disease Control and Prevention. (2015). Today’s heroin epidemic infographics. Retrieved from https://www.cdc.gov/vitalsigns/heroin/infographic.html
Centers for Disease Control and Prevention. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. Morbidity and Mortality Weekly Report Weekly, 64(50), 1378–82.
Centers for Disease Control and Prevention. (2016). Prescription opioid overdose data. Retrieved from https://www.cdc.gov/drugoverdose/data/overdose.html
Centers for Disease Control and Prevention. (2016). Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics.
Centers for Disease Control and Prevention. (2017). Heroin overdose data. Retrieved from https://www.cdc.gov/drugoverdose/data/heroin.html
Cicero, T. J., Ellis, M. S., Surratt, H. L., & Kurtz, S. P. (2014). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry, 71(7), 821–826.
Compton, W. M., Jones, C. M., & Baldwin, G. T. (2016). Relationship between nonmedical prescription-opioid use and heroin use. New England Journal of Medicine, 374(2), 154–163. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1508490#t=article
Coomber, R., & Sutton, C. (2006). Harm Reduction Digest 34: How quick to heroin dependence? Drug and Alcohol Review, 25(5), 463–471. Retrieved from https://onlinelibrary.wiley.com/doi/10.1080/09595230600883347/abstract
Darke, S. (2012). Pathways to heroin dependence: Time to re-appraise self-medication. Addiction, 108(4), 659–667.
Davis, C. (2016, March 1). “Over the counter” naloxone access, explained. The Network for Public Health Law. Retrieved from https://www.networkforphl.org/the_network_blog/2016/03/01/745/over_the_counter_naloxone_access_explained
Grattan, A., Sullivan, M. D., Saunders, K. W., Campbell, C. I., et al. (2012). Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substanceabuse. Annals of Family Medicine, 10(4), 304–311.
Jones, C. M., Baldwin, G. T., Manocchio, T., White, J. O., et al. (2016). Trends in methadone distribution for pain treatment, methadone diversion, and overdose deaths—United States, 2002–2014. Morbidity and Mortality Weekly Report, 65(26), 667–671.
Jones, C. M., Paulozzi, L. J., & Mack, K. A. (2014). Sources of prescription opioid pain relievers by frequency of past-year nonmedical use United States, 2008–2011. JAMA Internal Medicine, 174(5), 802–803.
Lankenau, S. E., Teti, M., Silva, K., Jackson Bloom, J., et al. (2012). Initiation into prescription opioid misuse amongst young injection drug users. International Journal of Drug Policy, 23(1), 37–44.
Ludden, J. (September 2, 2016). An even deadlier opioid, Carfentanil, is hitting the streets. National Public Radio. Retrieved from https://www.npr.org/sections/health-shots/2016/09/02/492108992/an-even-deadlier-opioid-carfentanil-is-hitting-the-streets
Mahoney, K. (2016, August 10). FDA supports greater access to naloxone to help reduce opioid overdose deaths. FDA Voice; US Food and Drug Administration. Retrieved from https://blogs.fda.gov/fdavoice/index.php/2016/08/fda-supports-greater-access-to-naloxone-to-help-reduce-opioid-overdose-deaths/
Miech, R., Johnston, L., O’Malley, P. M., Keyes, K. M., et al. (2015). Prescription opioids in adolescence and future opioid misuse. Pediatrics, 136(5), e1169–e1177.
National Institute on Drug Abuse. (2015). Prescription opioid use is a risk factor for heroin use. Retrieved from https://www.drugabuse.gov/publications/research-reports/relationship-between-prescription-drug-heroin-abuse/prescription-opioid-use-risk-factor-heroin-use
National Institutes of Health. (2017, January). Overdose death rates. Retrieved from https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
Noble, M., Treadwell, J. R., Tregear, S. J., Coates, V. H., et al. (2010). Opioids for long-term treatment of noncancer pain. The Cochrane Collaboration. Retrieved from https://www.cochrane.org/CD006605/SYMPT_opioids-long-term-treatment-noncancer-pain
Paulozzi, L. J., Budnitz, D. S., & Xi, Y. (2006). Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiology of Drug Safety, 15(9), 618–627.
Popovich, N. (2016, May 25). A deadly crisis: Mapping the spread of America’s drug overdose epidemic. Guardian. Retrieved from https://www.theguardian.com/society/ng-interactive/2016/may/25/opioid-epidemic-overdose-deaths-map
Rudd, R. A., Seth, P., David, F., & Scholl, L. (2016). Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Mortality and Morbidity Weekly Report, 65(50–51), 1445–1452.
Schwartz, A. (2015, April 25). Michael Botticelli is a drug czar who knows addiction firsthand. New York Times. Retrieved from https://www.nytimes.com/2015/04/26/us/michael-botticelli-is-a-drug-czar-who-knows-addiction-firsthand.html?_r=0
Senate Caucus on International Narcotics Control Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. 13-4795. Rockville, MD: SAMHSA, 2013.
Stobbe, M. (2016, December 9). A grim tally soars: More than 50,000 overdose deaths in US. STAT. Retrieved from https://www.statnews.com/2016/12/09/opoid-overdose-deaths-us/
Szalavitz, M. (2016, May 10). Opioid addiction is a huge problem, but pain prescriptions are not the cause. Scientific American. Retrieved from https://blogs.scientificamerican.com/mind-guest-blog/opioid-addiction-is-a-huge-problem-but-pain-prescriptions-are-not-the-cause/
Utah Department of Health. (2016). Prescription opioid deaths. Retrieved from https://health.utah.gov/vipp/pdf/RxDrugs/PDODeaths2015.pdf
Volkow, N. D. (2014, May 14). America’s addiction to opioids: Heroin and prescription drug abuse. National Institute of Drug Abuse. Retrieved from https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse
Vowles, K. E., McEntee, M. L., Julnes, P. S., Frohe, T., et al. (2015). Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Journal of Pain, 156(4), 569–576.
Whalen, J., & Spegele, B. (2016, June 23). The Chinese connection fueling America’s fentanyl crisis. Wall Street Journal. Retrieved from https://www.wsj.com/articles/the-chinese-connection-fueling-americas-fentanyl-crisis-1466618934.
White, P. F. (2017, March). What are the advantages of non-opioid analgesic techniques in the management of acute and chronic pain? Expert Opinions in Pharmacotherapeutics, 18(4), 329–333.
Whitworth, M. (2015, October 22). Can you really become addicted to a drug after just one hit? Vice. Retrieved from https://www.vice.com/en_us/article/reasons-why-you-cant-get-addicted-to-drugs-after-one-hit
Yokell, M. A., Delgado, M. K., Zaller, N. D., Wang, N. E., et al. (2014, December). Presentation of prescription and nonprescription opioid overdoses to US emergency departments. JAMA Internal Medicine, 174(12), 2034–2037. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1918924
If you choose to drink alcohol, you’re likely familiar with the relaxed, chatty buzz that may come early in the evening—and the slump that sometimes follows (the tiredness, the nausea, maybe the fear of what you posted online). If you’re drinking in school, you can learn how to get that buzz without the slump. For those who drink alcohol, this skill is key to a night—no, a lifetime—of positive experiences and few, if any, regrets.
What makes alcohol tricky to navigate? First, we need to understand how alcohol affects us—which in certain key respects is different from popular myth. With those basic concepts, we can choose to drink alcohol in ways that give us what we want from it.
Second, we all like to believe that we make our own choices, and to some extent, we do. But it’s complicated. A ton of research shows that our behavior, including what we drink, is highly dependent on what’s happening around us. In college, getting the alcohol buzz without the slump means grappling smartly with social dynamics, in addition to understanding the science of how alcohol affects us. This is especially relevant when you’re new to college, new to drinking, or both. (The minimum legal age for consuming alcohol in the US is 21.)
If you choose to drink alcohol, it may help you relax, socialize, and have fun—up to a point. Depending on what you drink, how much you drink, and how quickly or slowly you drink it, the alcohol level in your blood will rise to a certain level—let’s call it “peak buzz.”
For most people of average tolerance, peak buzz happens when your Blood Alcohol Content (BAC)—the concentration of alcohol in your bloodstream—approaches 0.06 percent. For most people, two to three drinks within an hour will have this effect. Some research indicates that 0.06 percent BAC is on the high side; you may find peak buzz comes at any point after 0.04 BAC.
Beyond that point—0.06 percent BAC—the enjoyable effects of alcohol decline and wear off. You may feel sleepy, flat, disconnected. You may get moody or sick, or make unwise decisions. From here, there’s no going back to peak buzz. Drinking more alcohol can only take you deeper into the slump and toward regret territory.
Explained by Dr. Jason Kilmer, associate professor of psychiatry and behavioral science, University of Washington:

“The biphasic aspect actually occurs within the brain. The brain center that inhibits our actions is the first to be affected (depressed) by alcohol. So without the inhibiting center the other areas somewhat go wild, and we feel uninhibited, etc. Later, the brain functions that allow us to act bolder and less shy also get depressed, and then we slump.” —Dr. Pierre-Paul Tellier, director of student health services at McGill University, Quebec
These buzz effects and slump effects in the chart are examples of how people may experience alcohol; the sequence of effects on each side of the chart is in no particular order.
The amount of alcohol you consume depends partly on what you’re drinking. Alcoholic beverages vary enormously in their alcohol content.
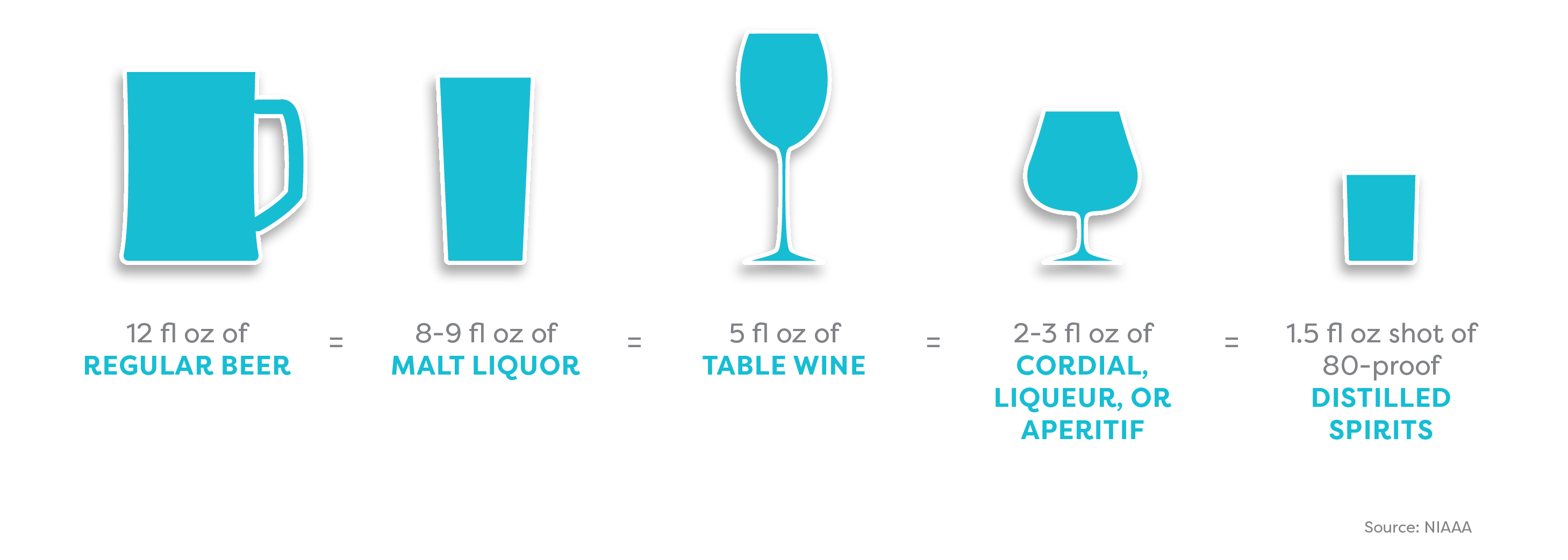
The amount of alcohol you consume also depends on the shape and size of your glass or cup. A standard serving size is unlikely to be whatever your new friend just ladled into that solo cup.
How to get the hang of serving sizes:
Try this size calculator (NIAAA)

The same size beverage can look very different depending on the size and shape of the cup or glass.
Think about pacing your drinking. Most people take about one hour to metabolize one standard drink. If you’ll be out for, say, four hours, and you plan to have three alcoholic drinks, you may decide to have one alcoholic drink per hour for the first three hours.
Pregaming—drinking before you go out—means you hit peak buzz earlier. If you keep drinking, your mood declines earlier too.
BAC calculators and charts help you estimate the number of standard drinks you can consume before your BAC reaches peak buzz (0.06 percent).
Example:
Woman (155 lb, 5’7″): 3 standard drinks in 3 hours
Man (155 lb, 5’7″): 3 ½ standard drinks in 3 hours
Check out this BAC chart (Yale University)
Or this one (Cleveland Clinic)
BAC charts and calculators are useful but limited tools:
They do not account for various other factors that may influence your alcohol tolerance (e.g., age, health, fatigue, medications, food consumed, and whether or not the environment is familiar).
You may need to adjust the BAC percentage to account for the amount of time you’re drinking.
Effective tools and tips for having fun and staying in control
Rethinking Drinking (info, tools, etc.): National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Handle your urge to drink and friends who offer: NIAAA
Calculators for alcohol content, calories, cost, etc.: NIAAA
Guides to the social dynamics around drinking alcohol: BestCollegeReviews.org
Stopping at the buzz: GoodTherapy.org
Best alcohol apps of 2016: Healthline.com
Article sources
Jason Kilmer, PhD, associate professor of psychiatry and behavioral science, University of Washington; assistant director of health and wellness for alcohol and other drug education, Division of Student Life, University of Washington.
Joan Masters, MEd, senior coordinator, Partners in Prevention, University of Missouri Wellness Resource Center; area consultant, The BACCHUS Network.
Ann Quinn-Zobeck, PhD, former senior director of BACCHUS initiatives and training, NASPA - Student Affairs Professionals in Higher Education (peer education initiatives addressing collegiate health issues at US colleges).
Pierre-Paul Tellier, MD, director of student health services, McGill University, Quebec.
Ryan Travia, MEd, associate dean of students for wellness, Babson College, Massachusetts; founding director, Office of Alcohol & Other Drug Services (AODS), Harvard University.
American College Health Association. American College Health Association–National College Health Assessment II: Reference Group Undergraduates Executive Summary Fall 2015. Hanover, MD: American College Health Association; 2016.
Borsari, B., & Carey, K. B. (2001). Peer influences on college drinking: A review of the research. Journal of Substance Abuse, 13, 391–424. Retrieved from https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.602.7429&rep=rep1&type=pdf
Borsari, B., & Carey, K. B. (2006). How the quality of peer relationships influences students’ alcohol use. Drug and Alcohol Review, 25(4), 361–370.
Crawford, L. A., & Novak, K. B. (2007). Resisting peer pressure: Characteristics associated with other-self discrepancies in college students’ levels of alcohol consumption. Journal of Alcohol and Drug Education, 51(1), 35–62.
Harrington, N. G. (1997). Strategies used by college students to persuade peers to drink. Southern Communication Journal, 62(3), 229–242. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/10417949709373057?journalCode=rsjc20
Kilmer, J., Cronce, J. M., & Logan, D. E. (2014). “Seems I’m not alone at being alone:” Contributing factors and interventions for drinking games in the college setting. The American Journal of Drug and Alcohol Abuse, 40(5), 411–414.
Neighbors, C., Lee, C. M., Lewis, M. A., Fossos, N., & Larimer, M. E. (2007). Are social norms the best predictor of outcomes among heavy-drinking college students? Journal of Studies on Alcohol and Drugs, 68, 556–565.
Neighbors, C., Jensen, M., Tidwell, J., Walter, T., Fossos, N., & Lewis, M. A. (2011). Social-norms interventions for light and nondrinking students. Group Processes & Intergroup Relations, 14(5), 651-669. doi: 10.1177/1368430210398014
Palmeri, J. M. (2016). Peer pressure and alcohol use among college students. Applied Psychology Opus, NYU Steinhardt. Retrieved from https://steinhardt.nyu.edu/appsych/opus/issues/2011/fall/peer
Perkins, H. W., Linkenbach, J. W., Lewis, M. A., & Neighbors, C. (2010). Effectiveness of social norms media marketing in reducing drinking and driving: A statewide campaign. Addictive Behaviors, 35, 866–874.
Seigel, S. (2011). The four-loko effect. Perspectives on Psychological Science, 6(4), 357–362.
Student Health 101 survey, July 2016.
Turner, J., Perkins, H.W., & Bauerle, J. (2008). Declining negative consequences related to alcohol misuse among students exposed to social norms marketing intervention on a college campus. Journal of American College Health, 57, 85−93.
Wechsler, H., Nelson, T. E., Lee, J. E., Seibring, M., Lewis, C., & Keeling, R. P. (2003). Perception and reality: A national evaluation of social norms marketing interventions to reduce college students’ heavy alcohol use. Journal of Studies on Alcohol, 64, 484–494.